
Figure 1. Skin Cancer Risk Factors. User-supplied image. © Copyright belongs to the original creator or publisher of the Skin Cancer Risk Factors. Used for reference/educational purposes only.
Skin cancer is the most commonly diagnosed cancer in Australia, and many people don’t realise they may fall into a high-risk category. Understanding your personal risk factors can help you take proactive steps toward early detection and prevention.
Below is a simple guide outlining what makes someone high-risk, why these factors matter, and the potential outcomes if risk isn’t managed early.
What Makes Someone High-Risk for Skin Cancer?
1. Fair or Light Skin
People with fair skin, light eyes, or red/blonde hair naturally have less melanin, reducing the skin’s ability to block UV radiation.
Outcome: Faster sunburn, increased DNA damage, and a significantly higher lifetime risk of melanoma and non-melanoma skin cancers.
2. Family History of Melanoma or Skin Cancers
Having a first-degree relative with melanoma increases a person’s own risk due to shared genetics and similar environmental exposures.
Outcome: Earlier onset cancers and a higher chance of developing multiple lesions over time.
3. History of Sunburns or Tanning
Childhood blistering sunburns or regular tanning (including solarium use) dramatically increase lifetime melanoma risk.
Outcome: The skin develops cumulative UV damage, leading to premature ageing, DNA mutations, and a higher melanoma incidence.
4. High UV Exposure or Outdoor Lifestyle
Living in Australia—particularly Queensland—means exposure to some of the world’s highest UV levels. Outdoor workers and athletes are at increased risk.
Outcome: Accelerated skin cell damage and a greater chance of both melanomas and keratinocyte cancers.
5. Numerous Moles or Atypical Moles
Having more than 50 moles or irregularly shaped/dysplastic moles increases the chance that one may become cancerous.
Outcome: Requires regular dermoscopic monitoring, as melanoma may develop in an existing mole or appear as a new lesion.
6. Age Over 50
Skin cancer risk increases as UV damage accumulates over decades.
Outcome: Higher likelihood of basal cell carcinoma (BCC), squamous cell carcinoma (SCC), and melanoma.
7. Suppressed Immune System
People on immunosuppressive medications (e.g., after organ transplant) or with medical conditions affecting immunity are at significantly higher risk.
Outcome: Faster-growing and more aggressive skin cancers that require close medical follow-up.
8. Previous Skin Cancer
Once you’ve had any form of skin cancer, your chance of developing another increases.
Outcome: Lifelong need for professional skin checks and ongoing surveillance.
Why Identifying Risk Matters
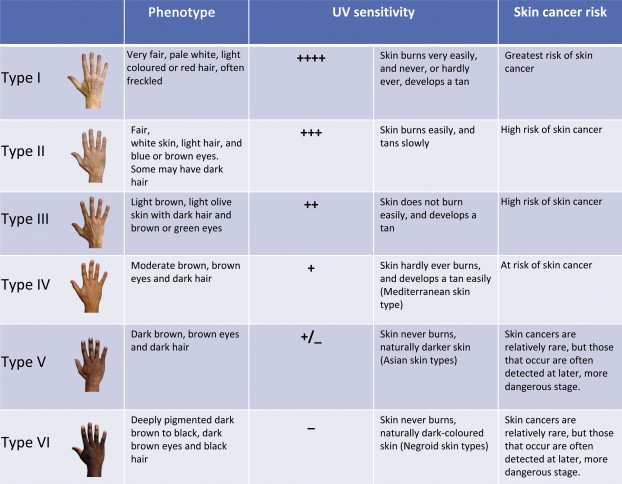
Figure 2. Skin Type & UV Sensitivity. User-supplied image. © Copyright belongs to the original creator or publisher of the Skin Type & UV Sensitivity. Used for reference/educational purposes only.
Understanding your risk factors allows for:
- Earlier detection — improving survival outcomes for melanoma.
- Better prevention — sun protection and behaviour changes.
- Personalised monitoring — including dermoscopy and AI-assisted skin imaging.
- Reduced treatment severity — early lesions require simpler, less invasive procedures.
If you identify with any of the above factors, regular full-body skin checks every 6–12 months are recommended.

